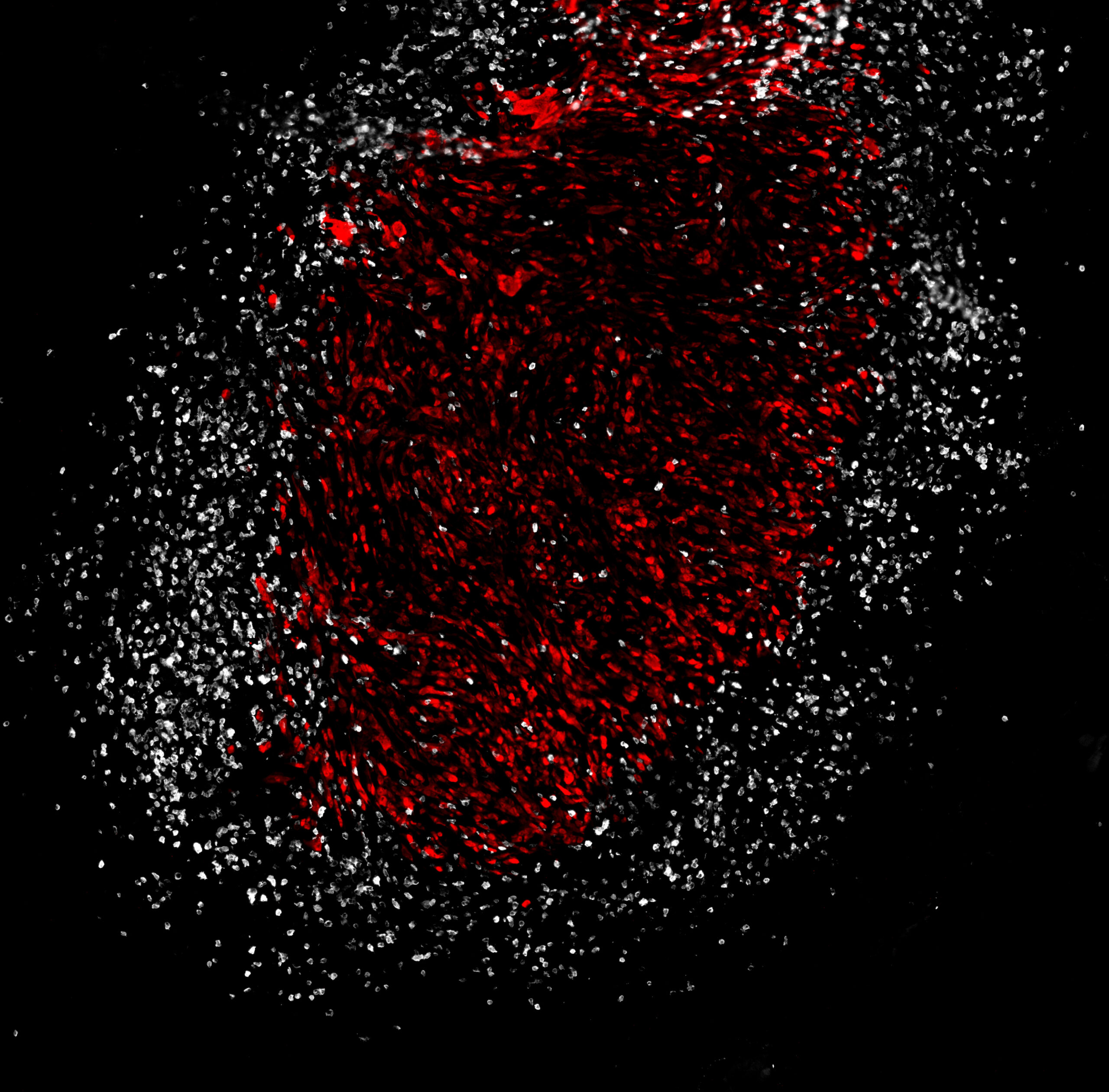
Combination checkpoint blockade therapy (CBT) employing anti-CTLA-4 and anti-PD-1 antibodies has been shown to significantly improve overall survival of patients with non-small cell lung cancer (NSCLC). But the treatment only benefits about a third of all patients. This is mainly due to the many mechanisms by which tumor cells directly and indirectly suppress the anti-tumor immune responses engaged by CBT. These include signaling pathways activated within cancer cells that manipulate the immune landscape of the tumor’s internal microenvironment. Researchers led by Ludwig MIT’s Stefani Spranger reported in a January issue of Cancer Immunology Research a novel mechanism by which NSCLC tumors exclude effector T cells from their core. They found that expression of the developmental transcription factor SOX2 by NSCLC cells induces expression of the chemotactic factor CCL2 and boosts recruitment of regulatory T cells (Tregs) into the tumor that express the regulatory protein GITR at high levels on their surface. These Tregs alter the tumor vasculature to exclude CD8+ T cells from the tumor core, promoting resistance to CBT. Depleting GITR+ Tregs in mouse models improved CD8+ T cell infiltration of the tumor core and sensitized tumors to CBT, suggesting a strategy to improve NSCLC responses to immunotherapy.
Lung cancer-intrinsic SOX2 expression mediates resistance to checkpoint blockade therapy by inducing Treg cell-dependent CD8+ T-cell exclusion
Cancer Immunology Research, 2025 January 2